Menu
Search
- Locations
- About
-
Services
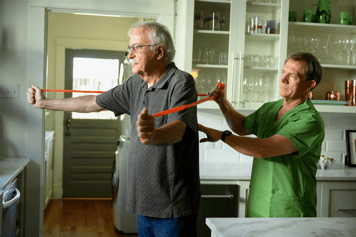
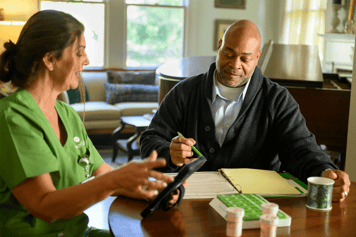
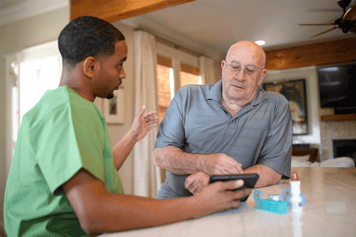
Home Health Care
Skilled nursing, therapy and other services to help with illness, injury or surgery Is Home Health the Answer? Home Health Care Services Home Health Care Team Home Health FAQs Specialty Programs Complete Guide to Home HealthHospice Care
Physical, emotional and spiritual care at the end of life Hospice Care Services Our Hospice Philosophy Hospice Care Team Hospice FAQs Specialty Programs Volunteers & Donations Complete Guide to Hospice CarePalliative Care
Relief from pain and symptoms at any stage of a serious illness Palliative Care Services Palliative Care Team Palliative Care FAQsHospital-Level and Skilled Nursing Care at Home
Contessa, an Amedisys company, enables a new standard of care with provider partners and payors to allow patients to be treated for serious health conditions at home Innovative Solutions Current Partnerships Resources - Resources
-
Healthcare
Providers